VitalStream® for the ICU
Elevate care for your most critical patients with the only wireless, noninvasive hemodynamic monitor.
VitalStream is a wireless, noninvasive hemodynamic monitoring system that empowers you with the continuous data needed to help reduce complications and ICU length of stay (LOS). VitalStream uses AI algorithms and patented Pulse Decomposition Analysis to continuously measure over 20 vital sign parameters including blood pressure, cardiac output, stroke volume, systemic vascular resistance, fluid status and more.
The device can be fit, calibrated and monitoring within 90 seconds and uses an innovative low-pressure finger sensor that can be comfortably worn by awake patients throughout their entire hospital stay. VitalStream eliminates monitoring blind spots and provides you with the information you need to accurately assess volume status and titrate pressors or inotropes.

Clinically validated with patients on vasoactive drugs
 “VitalStream is the only device that gives you this level of continuous hemodynamic information and is completely detached from a monitor. The patient can just walk around with a wrist band.” ~ Aniket Rali, MD, FACC, FCCP, Advanced Heart Failure and Transplantation, Critical Care Medicine, Assistant Professor of Medicine and Anesthesiology, Vanderbilt University Medical Center
“VitalStream is the only device that gives you this level of continuous hemodynamic information and is completely detached from a monitor. The patient can just walk around with a wrist band.” ~ Aniket Rali, MD, FACC, FCCP, Advanced Heart Failure and Transplantation, Critical Care Medicine, Assistant Professor of Medicine and Anesthesiology, Vanderbilt University Medical Center
 “VitalStream literally gives beat-to-beat blood pressure data so nothing is lost.” ~ Youngoon Kwon, MD, Director of Cardiac ICU/Inpatient Services at Harborview Medical Center, Associate Director of Cardiac ICU University of Washington Medical Center
“VitalStream literally gives beat-to-beat blood pressure data so nothing is lost.” ~ Youngoon Kwon, MD, Director of Cardiac ICU/Inpatient Services at Harborview Medical Center, Associate Director of Cardiac ICU University of Washington Medical Center
Why noninvasive hemodynamic patient monitoring in the ICU?
Even short periods of hypotension are associated with kidney and myocardial injury.3-5
of patients on IV fluid therapy suffer complications due to incorrect fluid administration.8
Spot checked blood pressure can lead to delayed event recognition and treatment, which can lead to adverse outcomes.5
Fluid overload is associated with a 29% increase in length of stay and a $15,334 increase in hospital costs per patient.9, 10
Hemodynamic instability is the second most common cause of ICU readmission at 31%.6 And hospital death rates are significantly higher for patients who are readmitted. 7
Deliver the safest care for your sickest patients
Gain insights to tailor fluid administration with the touch of a button.
Reduce the risk of complications and infections from invasive lines.
Get near real-time data and beat-by-beat insights into hemodynamic parameters for early detection of clinical decompensation.
Enable early ambulation with a wire-free monitoring experience.
Streamline your workflow
A one-size-fits-all finger sensor for streamlined application.
Fit, calibrate and monitor within 90 seconds for expedited set-up.
Reposition patients without cumbersome wires in your way and there’s no need to re-zero upon position changes.
Eliminate manual vital signs charting and transcription errors with EHR or monitoring system integration.
Reduce hospital costs
A cost-effective alternative at about 1/10 the cost of other ICU monitoring systems.
A comfortable finger sensor that can be worn for up to 12 days and removed when needed.
Easily portable from one floor to the next for seamless monitoring and expedited transfer to a lower cost bed.
Take the guess work out of fluid assessment to drive better outcomes
Incorrect fluid administration can result in delayed recovery, increased length of stay, complications and costs. Around 50% of fluid boluses fail to improve cardiac output and perfusion.11 And fluid balance is an independent risk factor for 28-day mortality acute kidney injury.12
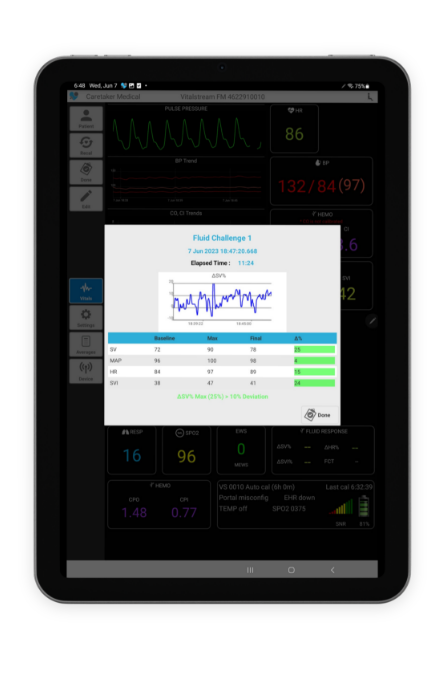
VitalStream offers near real-time continuous hemodynamic data that provides you with the information needed to accurately assess a patient’s fluid status. The fluid response feature allows you to quickly and easily identify if a patient is fluid responsive with the touch of a button. The percent of change calculations are done for you and fluid response is visually indicated.
Achieve SEP-1 reimbursement and improve sepsis outcomes
A 2022 study in CHEST showed that completion of all SEP-1 compliance elements is associated with a lower 30-day mortality rate a shorter LOS. 13 The sepsis treatment guidelines require 30 m/kg of crystalloid fluid to be given within three hours of sepsis identification and repeat volume assessment within six. But for some patients administering fluid or more fluid could be disastrous.
In the US, V5.14 of the Specifications Manual for National Hospital Inpatient Quality Measures includes guidance that you can document cardiac output, cardiac index, stroke volume or stroke volume index if a lesser amount of no fluids are ordered and still achieve SEP-1 measure compliance and reimbursement.
VitalStream enables you to quickly assess a patients fluid status and provides you with continuous CO, CI, SV and SVI data so you can the best treatment decisions for your patients.
Untether your patients for easier early mobilization
Studies show that early mobilization in the intensive care unit can have many positive effects including decreases in muscle atrophy, mechanical ventilation duration and length of stay.14 But timing is critical. Delayed mobilization of even a few days, can greatly impact outcomes. 15
VitalStream is the only FDA approved and clinically-validated continuous cardiac output monitor that eliminates cumbersome wires. The wearable formfactor, easily removable finger sensor and wireless Bluetooth capabilities all help enable easier early ambulation and therefore improved outcomes.

The latest news, webinars and case studies

Caretaker Medical Receives Inaugural Healthcare Tech Innovation Award and $200,000 Grant from Medical Society of D.C.
WASHINGTON, DC, UNITED STATES, April 2, 2025 /EINPresswire.com/ -Caretaker Medical is honored to announce it has been awarded the Healthcare Technology Innovation Award, along with…

VitalStream offers continuous hemodynamic monitoring solution amid IV fluid shortage
Philadelphia, PA – October 9, 2024 – Caretaker Medical, a pioneer in advanced hemodynamic monitoring technology, is highlighting the critical role of its VitalStream solution…

BP cuff, A-line or VitalStream noninvasive hemodynamic monitor?
Should you use a blood pressure cuff, arterial line or VitalStream to monitor your perioperative patients? Learn the about the strengths and weaknesses of each….
Request a demo
See how VitalStream can improve the continuous hemodynamic monitoring experience for you and your patients.

- Kwon Y, Stafford PL, Enfield K, Mazimba S, Baruch MC. Continuous Noninvasive Blood Pressure Monitoring of Beat-By-Beat Blood Pressure and Heart Rate Using Caretaker Compared With Invasive Arterial Catheter in the Intensive Care Unit. J Cardiothorac Vasc Anesth. 2022 Jul;36(7):2012-2021. doi: 10.1053/j.jvca.2021.09.042. Epub 2021 Oct 1. PMID: 34666928; PMCID: PMC8971137.
- Khanna AK, Garcia JO, Saha AK, Harris L, Baruch M, Martin RS. Agreement between cardiac output estimation with a wireless, wearable pulse decomposition analysis device and continuous thermodilution in post cardiac surgery intensive care unit patients. J Clin Monit Comput. 2023 Jul 17. doi: 10.1007/s10877-023-01059-5. Epub ahead of print. PMID: 37458916.
- Sessler DI, Bloomstone JA, Aronson S, Berry C, Gan TJ, Kellum JA, Plumb J, Mythen MG, Grocott MPW, Edwards MR, Miller TE; Perioperative Quality Initiative-3 workgroup; POQI chairs; Miller TE, Mythen MG, Grocott MP, Edwards MR; Physiology group; Preoperative blood pressure group; Intraoperative blood pressure group; Postoperative blood pressure group. Perioperative Quality Initiative consensus statement on intraoperative blood pressure, risk and outcomes for elective surgery. Br J Anaesth. 2019 May;122(5):563-574. doi: 10.1016/j.bja.2019.01.013. Epub 2019 Feb 27. PMID: 30916004.
- Josep Solà*, Martin Proença, Fabian Braun, Nicolas Pierrel, Yan Degiorgis, Christophe Verjus, Mathieu Lemay, Mattia Bertschi and Patrick Schoettker. Continuous non-invasive monitoring of blood pressure in the operating room: a cuffless optical technology at the fingertip. DOI 10.1515/cdbme-2016-0060
- Salmasi V, Maheshwari K, Yang D, Mascha EJ, Singh A, Sessler DI, Kurz A. Relationship between Intraoperative Hypotension, Defined by Either Reduction from Baseline or Absolute Thresholds, and Acute Kidney and Myocardial Injury after Noncardiac Surgery: A Retrospective Cohort Analysis. Anesthesiology. 2017 Jan;126(1):47-65. doi:10.1097/ALN.0000000000001432. PMID: 27792044. https://pubmed.ncbi.nlm.nih.gov/27792044/
- Balshi AN, Huwait BM, Noor ASN, Alharthy AM, Madi AF, Ramadan OE, Balahmar A, Mhawish HA, Marasigan BR, Alcazar AM, Rana MA, Aletreby WT. Modified Early Warning Score as a predictor of intensive care unit readmission within 48 hours: a retrospective observational study. Rev Bras Ter Intensiva. 2020 Jun;32(2):301-307. doi: 10.5935/0103-507x.20200047. Epub 2020 Jul 13. PMID: 32667433; PMCID: PMC7405753.
- Andrew L. Rosenberg, Charles Watts, Patients Readmitted to ICUs: A Systematic Review of Risk Factors and Outcomes, Chest, Volume 118, Issue 2, 2000, Pages 492-502, ISSN 0012-3692, https://doi.org/10.1378/chest.118.2.492.
- Institute for Health and Care Excellence. Intravenous fluid therapy in adults in hospital – clinical guideline (CG174). https://www.nice.org.uk/guidance/cg174. Published December 2013. Updated May 2017. Accessed (August 20, 2020).
- Magee G, Zbrozek A. Fluid overload is associated with increases in length of stay and hospital costs: pooled analysis of data from more than 600 US hospitals. Clinicoecon Outcomes Res. 2013 Jun 26;5:289-96. doi: 10.2147/CEOR.S45873. PMID: 23836999; PMCID: PMC3699028.
- Child, Debra & Cao, Zhun & Seiberlich, Laura & Brown, Harold & Greenberg, Jordan & Swanson, Anne & Sewall, Martha & Robinson, Scott. (2015). The costs of fluid overload in the adult intensive care unit: Is a small-volume infusion model a proactive solution?. ClinicoEconomics and outcomes research : CEOR. 7. 1-8. 10.2147/CEOR.S72776.
- Michard F, Teboul JL. Predicting fluid responsiveness in ICU patients: a critical analysis of the evidence. Chest. 2002;121(6):2000–8. doi: 10.1378/chest.121.6.2000.
- Patil VP, Salunke BG. Fluid Overload and Acute Kidney Injury. Indian J Crit Care Med. 2020 Apr;24(Suppl 3):S94-S97. doi: 10.5005/jp-journals-10071-23401. PMID: 32704211; PMCID: PMC7347067.
- Douglas IS, Alapat PM, Corl KA, Exline MC, Forni LG, Holder AL, Kaufman DA, Khan A, Levy MM, Martin GS, Sahatjian JA, Seeley E, Self WH, Weingarten JA, Williams M, Hansell DM. Fluid Response Evaluation in Sepsis Hypotension and Shock: A Randomized Clinical Trial. Chest. 2020 Oct;158(4):1431-1445. doi: 10.1016/j.chest.2020.04.025. Epub 2020 Apr 27. PMID: 32353418; PMCID: PMC9490557. https://pubmed.ncbi.nlm.nih.gov/32353418/
- Gopala Krishna Alaparthi, Aishwarya Gatty, Stephen Rajan Samuel, Sampath Kumar Amaravadi, "Effectiveness, Safety, and Barriers to Early Mobilization in the Intensive Care Unit", Critical Care Research and Practice, vol. 2020, Article ID 7840743, 14 pages, 2020. https://doi.org/10.1155/2020/7840743
- Schweickert WD, Patel BK, Kress JP. Timing of early mobilization to optimize outcomes in mechanically ventilated ICU patients. Intensive Care Med. 2022 Oct;48(10):1305-1307. doi: 10.1007/s00134-022-06819-6. Epub 2022 Aug 4. PMID: 35925320; PMCID: PMC10139766. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10139766/
