VitalStream® for Perioperative Care
Make better treatment decisions throughout the entire perioperative continuum with continuous hemodynamic data.
VitalStream is a wireless, noninvasive advanced hemodynamic monitor that can seamlessly bridge monitoring gaps throughout perioperative care. The innovative low-pressure finger sensor can be comfortably worn by conscious patients. This allows VitalStream to easily be placed on patients in preop so you can get baseline readings and save valuable time in the OR.
VitalStream uses AI algorithms and patented Pulse Decomposition analysis to measure continuous blood pressure (BP), cardiac output (CO), systemic vascular resistance (SVR), cardiac power (CP) and other physiological parameters. It can provide immediate insights in
near real-time for early detection of decompensation and enable early intervention.

Clinically validated with patients on vasoactive drugs
 "We’ve abandoned using arterial lines in transcatheter value surgery. VitalStream saves time, is safer and we have accurate readings.” ~ Zain Khalpey, MD, Cardiothoracic Surgeon, Director of Artificial Heart, MCS & ECMO, Chief Medical AI Officer (Network Director) at Honor Health
"We’ve abandoned using arterial lines in transcatheter value surgery. VitalStream saves time, is safer and we have accurate readings.” ~ Zain Khalpey, MD, Cardiothoracic Surgeon, Director of Artificial Heart, MCS & ECMO, Chief Medical AI Officer (Network Director) at Honor Health
 “A noninvasive and clinically validated technology opens the door for use in more mobile patients and can extend hemodynamic monitoring to other units so they can be more closely monitored.” ~ Ashish K. Khanna, MD, Intensivist and Anesthesiologist, and Vice Chair of Research at the Atrium Health Wake Forest Baptist Medical Center
“A noninvasive and clinically validated technology opens the door for use in more mobile patients and can extend hemodynamic monitoring to other units so they can be more closely monitored.” ~ Ashish K. Khanna, MD, Intensivist and Anesthesiologist, and Vice Chair of Research at the Atrium Health Wake Forest Baptist Medical Center
 “I’ve seen less incidence of renal failure or impairment because we are making better decisions before operating, in the operation and after in the ICU.” ~ Zain Khalpey, MD, Cardiothoracic Surgeon, Director of Artificial Heart, MCS & ECMO, Chief Medical AI Officer (Network Director) at Honor Health
“I’ve seen less incidence of renal failure or impairment because we are making better decisions before operating, in the operation and after in the ICU.” ~ Zain Khalpey, MD, Cardiothoracic Surgeon, Director of Artificial Heart, MCS & ECMO, Chief Medical AI Officer (Network Director) at Honor Health
 “My use of the VitalStream monitor in the OR demonstrates compelling benefits in continuous, accurate and actionable data.” ~ Karen Boretsky, MD, Senior Associate in Perioperative Anesthesia at Boston Children’s Hospital, Assistant Professor of Anesthesia at Harvard Medical School
“My use of the VitalStream monitor in the OR demonstrates compelling benefits in continuous, accurate and actionable data.” ~ Karen Boretsky, MD, Senior Associate in Perioperative Anesthesia at Boston Children’s Hospital, Assistant Professor of Anesthesia at Harvard Medical School
Traditional blood pressure monitoring
Avoid dangerous blind spots in your next surgery
Traditional cuff-based monitoring only gives you intermittent snap shots of a patient’s blood pressure. That means, in a 90-minute surgery with spot checks every 5 minutes, you are missing a staggering 72 minutes (4,320 seconds) of critical data or 80% of the procedure! And even brief hypotensive events can trigger serious perioperative complications including acute kidney injury (AKI) and myocardial infarction (MI). 3,4
VitalStream provides continuous, beat-by-beat blood pressure measurements to eliminate blind spots throughout the entire perioperative continuum.

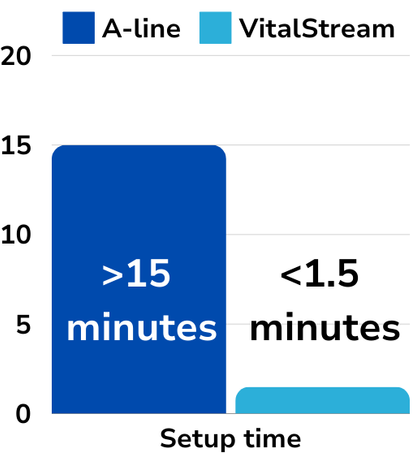
Reduce monitoring set up time by over 90%!
Reclaim over 13 minutes in your next surgery
Traditional radial artery setup for blood pressure monitoring can take a frustrating 15+ minutes. That’s precious time lost when minutes matter. This time can add up and translate into significant costs for your hospital. Improved OR efficiency can potentially improve on-time starts and lower operating costs.
VitalStream noninvasive hemodynamic monitor can be set up in preop in just 60-90 seconds, measures central aortic pressures so there’s no need to level or zero upon position changes, and eliminates cumbersome wires.
Why continuous hemodynamic monitoring for perioperative care?
Even short periods of hypotension are associated with kidney and myocardial injury.3,4
of non-cardiac surgical patients experience an intraoperative hypotensive event.4
Spot checked blood pressure can lead to delayed event recognition and treatment, which can lead to adverse outcomes.3
Postoperative complications are the third most common cause of death in the world.5
Enhance patient safety
Gain insights to tailor fluid administration with the touch of a button.
Reduce the risk of perioperative complications and infections from invasive lines.
Get near real-time data and beat-by-beat insights into hemodynamic parameters for early detection of cardiovascular insufficiency.
Enable early ambulation after surgery with a wire-free monitoring experience.
Streamline your workflow for more efficient care
A one-size-fits-all finger sensor for streamlined application.
Fit, calibrate and monitor within 90 seconds for expedited pre op set-up.
Reposition patients without cumbersome wires in your way and there’s no need to re-zero upon position changes.
Easily portable from one floor to the next for seamless monitoring throughout a patient’s hospital stay.
Eliminate manual vital signs charting and transcription errors with EHR or monitoring system integration.
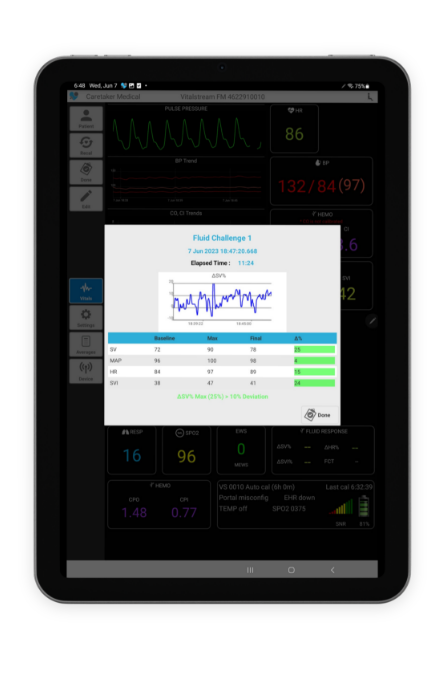
Tailor fluid administration for improved outcomes
Incorrect fluid administration can be disastrous and result in delayed recovery, increased length of stay, complications and costs. Positive and negative fluid balance increases the occurrence and progression of AKI after cardiac surgery.6 And volume overload is one of the five most common reasons for both acute and delayed readmission after cardiac surgery.7
VitalStream’s fluid response feature allows you to quickly and easily identify if a patient is fluid responsive. All you have to do is start and stop the timer with a push of a button. The percent of change calculations are done for you.
Enable early mobilization without sacrificing clinical insights

Early postoperative mobilization is a central tenent of Enhanced Recovery After Surgery (ERAS). Good compliance with ERAS pathway implementation is associated with improved outcomes including a reduced risk of complications, LOS and costs. The majority of ERAS guidelines strongly recommend early postoperative mobilization.8
The VitalStream noninvasive hemodynamic monitor eliminates wires to untether your patients. It enables early ambulation after surgery without sacrificing advanced blood pressure and vital signs monitoring.
Request a demo
See how VitalStream can improve the continuous hemodynamic monitoring experience for you and your patients.

The latest news, webinars and case studies

VitalStream offers continuous hemodynamic monitoring solution amid IV fluid shortage
Philadelphia, PA – October 9, 2024 – Caretaker Medical, a pioneer in advanced hemodynamic monitoring technology, is highlighting the critical role of its VitalStream solution…

BP cuff, A-line or VitalStream noninvasive hemodynamic monitor?
Should you use a blood pressure cuff, arterial line or VitalStream to monitor your perioperative patients? Learn the about the strengths and weaknesses of each….

SEP-1 became pay-for-performance in 2024 – Is your hospital ready?
Sepsis is one of the most deadly and costly conditions. But now poor SEP-1 performance could be even costlier for your hospital. Starting January 1,…
- Kwon Y, Stafford PL, Enfield K, Mazimba S, Baruch MC. Continuous Noninvasive Blood Pressure Monitoring of Beat-By-Beat Blood Pressure and Heart Rate Using Caretaker Compared With Invasive Arterial Catheter in the Intensive Care Unit. J Cardiothorac Vasc Anesth. 2022 Jul;36(7):2012-2021. doi: 10.1053/j.jvca.2021.09.042. Epub 2021 Oct 1. PMID: 34666928; PMCID: PMC8971137.
- Khanna AK, Garcia JO, Saha AK, Harris L, Baruch M, Martin RS. Agreement between cardiac output estimation with a wireless, wearable pulse decomposition analysis device and continuous thermodilution in post cardiac surgery intensive care unit patients. J Clin Monit Comput. 2023 Jul 17. doi: 10.1007/s10877-023-01059-5. Epub ahead of print. PMID: 37458916.
- Salmasi V, Maheshwari K, Yang D, Mascha EJ, Singh A, Sessler DI, Kurz A. Relationship between Intraoperative Hypotension, Defined by Either Reduction from Baseline or Absolute Thresholds, and Acute Kidney and Myocardial Injury after Noncardiac Surgery: A Retrospective Cohort Analysis. Anesthesiology. 2017 Jan;126(1):47-65. doi:
10.1097/ALN.0000000000001432. PMID: 27792044. - Sessler DI, Bloomstone JA, Aronson S, Berry C, Gan TJ, Kellum JA, Plumb J, Mythen MG, Grocott MPW, Edwards MR, Miller TE; Perioperative Quality Initiative-3 workgroup; POQI chairs; Miller TE, Mythen MG, Grocott MP, Edwards MR; Physiology group; Preoperative blood pressure group; Intraoperative blood pressure group; Postoperative blood pressure group. Perioperative Quality Initiative consensus statement on intraoperative blood pressure, risk and outcomes for elective surgery. Br J Anaesth. 2019 May;122(5):563-574. doi: 10.1016/j.bja.2019.01.013. Epub 2019 Feb 27. PMID: 30916004.
- Nepogodiev D,et al. Global burden of postoperative death. Lancet 2019. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)33139-8/fulltext
- Chen X, Xu J, Li Y, Shen B, Jiang W, Luo Z, Wang C, Teng J, Ding X, Lv W. The Effect of Postoperative Fluid Balance on the Occurrence and Progression of Acute Kidney Injury After
Cardiac Surgery. J Cardiothorac Vasc Anesth. 2021 Sep;35(9):2700-2706. doi: 10.1053/j.jvca.2020.10.007. Epub 2020 Oct 10. PMID: 33158712. https://www.jcvaonline.com/article/S1053-0770(20)31121-6/fulltext - Iribarne A, Chang H, Alexander JH, Gillinov AM, Moquete E, Puskas JD, Bagiella E, Acker MA, Mayer ML, Ferguson TB, Burks S, Perrault LP, Welsh S, Johnston KC, Murphy M,
DeRose JJ, Neill A, Dobrev E, Baio KT, Taddei-Peters W, Moskowitz AJ, O'Gara PT. Readmissions after cardiac surgery: experience of the National Institutes of Health/Canadian
Institutes of Health research cardiothoracic surgical trials network. Ann Thorac Surg. 2014 Oct;98(4):1274-80. doi: 10.1016/j.athoracsur.2014.06.059. Epub 2014 Aug 28. PMID:
25173721; PMCID: PMC4186890. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4186890/ - Tazreean R, Nelson G, Twomey R. Early mobilization in enhanced recovery after surgery pathways: current evidence and recent advancements. J Comp Eff Res. 2022 Feb;11(2):121-
129. doi: 10.2217/cer-2021-0258. Epub 2022 Jan 20. PMID: 35045757.
