VitalStream® for Emergency Room Care
When minutes matter, fast access to the right hemodynamic data can make a difference.
VitalStream is a wireless, noninvasive hemodynamic monitor that enables quick assessment and intervention in the ED. The monitoring device can be fit, calibrated and monitoring within 90 seconds and uses an innovative low-pressure finger sensor that can be comfortably worn by patients upon arrival.
VitalStream uses AI algorithms and patented Pulse Decomposition analysis to continuously measure blood pressure (BP), cardiac output (CO), stroke volume (SV), systemic vascular resistance (SVR), fluid status and other physiological parameters. The continuous data removes monitoring blind spots and provides you with the information you need to accurately assess volume status.

Noninvasive blood pressure monitoring with clinically-validated accuracy
 "VitalStream gives me instant hemodynamic feedback from a fluid bolus. This helps me tailor patient care instead of blindly pushing fluids which can be detrimental to patients as well as hospital costs." ~ Damon Kuehl, MD, Vice Chair Emergency Medicine at Virginia Tech Carilion School of Medicine
"VitalStream gives me instant hemodynamic feedback from a fluid bolus. This helps me tailor patient care instead of blindly pushing fluids which can be detrimental to patients as well as hospital costs." ~ Damon Kuehl, MD, Vice Chair Emergency Medicine at Virginia Tech Carilion School of Medicine
 “In some scenarios, you absolutely need to have more than blood pressure in your armamentarium. Treating hypotension solely based on blood pressure may send you the wrong way.” ~ Ashish K. Khanna, MD, Intensivist and Anesthesiologist, and Vice Chair of Research at the Atrium Health Wake Forest Baptist Medical Center
“In some scenarios, you absolutely need to have more than blood pressure in your armamentarium. Treating hypotension solely based on blood pressure may send you the wrong way.” ~ Ashish K. Khanna, MD, Intensivist and Anesthesiologist, and Vice Chair of Research at the Atrium Health Wake Forest Baptist Medical Center
 “Monitoring technologies have traditionally been restricted to operating rooms and intensive care units, but the need for assessing and adjusting fluid status in other care settings like the ER is often critical. A clinically validated, noninvasive and wireless device such as VitalStream can be used quickly and effectively in other areas of the hospital and can therefore help improve patient care.” ~ Irwin Gratz, DO, Anesthesiologist at Cooper University Health Care
“Monitoring technologies have traditionally been restricted to operating rooms and intensive care units, but the need for assessing and adjusting fluid status in other care settings like the ER is often critical. A clinically validated, noninvasive and wireless device such as VitalStream can be used quickly and effectively in other areas of the hospital and can therefore help improve patient care.” ~ Irwin Gratz, DO, Anesthesiologist at Cooper University Health Care
Why continuous hemodynamic monitoring in the ER?
Spot checked blood pressure can lead to delayed event recognition and treatment, which can lead to adverse outcomes.3
of patients on IV fluid therapy suffer complications due to incorrect fluid administration.5
of adverse events and preventable deaths occur in unmonitored beds.4
Fluid overload is associated with a 29% increase in length of stay and a $15,334 increase in hospital costs per patient.6,7
Streamline your workflow so you can intervene with speed
A one-size-fits-all finger sensor for streamlined application.
Fit, calibrate and monitor within 90 seconds for expedited set-up.
Easily portable from one floor to the next for seamless monitoring from arrival to discharge.
Eliminate manual vital signs charting and transcription errors with EHR or monitoring system integration.
Deliver the safest emergency care
Eliminate monitoring blind spots with near real-time continuous vital signs data for immediate detection of cardiovascular insufficiency.
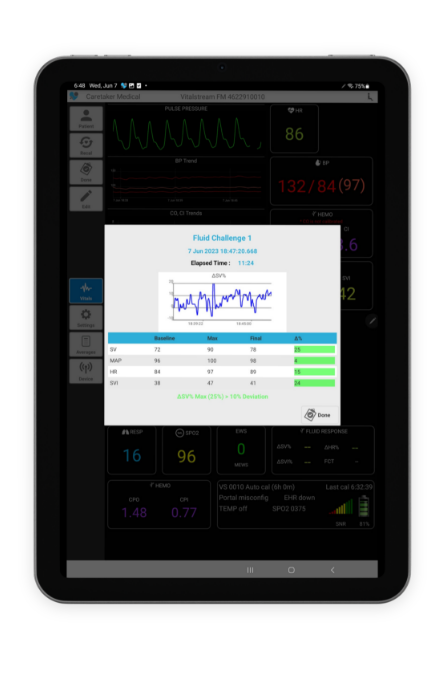
Gain insights to tailor fluid administration with the touch of a button.
Personalize fluid administration for improved outcomes
Incorrect fluid administration can result in delayed recovery, increased length of stay, complications and costs. That’s why accurate assessment of a patient’s volume status and knowing if they respond to a fluid challenge with an increase in cardiac output is essential. But unfortunately, there has been limited technology that can quickly provide the right data the ER setting. This and the fast paced nature of the ER, may contribute to most fluid decisions being made empirically.8
VitalStream provides you with real-time, continuous vital signs data that equips you with the information needed to accurately identify whether a patient is fluid responsive and if the issue involves contractility or afterload. The fluid response feature allows you to quickly and easily identify if a patient is fluid responsive. All you have to do is start and stop the timer with a push of a button. The percent of change calculations are done for you.
Achieve SEP-1 reimbursement and improve sepsis outcomes
Sepsis is associated with over 850,000 emergency room visits a year and about 80% of sepsis patients receive initial care in the emergency department.9 The sepsis treatment guidelines require 30 m/kg of crystalloid fluid to be given within three hours of sepsis identification and repeat volume assessment within six. But for some patients administering fluid or more fluid could be disastrous.
In the US, V5.14 of the Specifications Manual for National Hospital Inpatient Quality Measures includes guidance that you can document cardiac output (CO), cardiac index (CI), stroke volume (SV) or stroke volume index (SVI) if a lesser amount or no fluids are ordered and still achieve SEP-1 measure compliance and reimbursement.
VitalStream enables you to quickly assess a patient’s volume status upon arrival in the ED and provides you with continuous CO, CI, SV and SVI data so you can the best treatment decisions for your patients.
The latest news, webinars and case studies

Caretaker Medical Receives Inaugural Healthcare Tech Innovation Award and $200,000 Grant from Medical Society of D.C.
WASHINGTON, DC, UNITED STATES, April 2, 2025 /EINPresswire.com/ -Caretaker Medical is honored to announce it has been awarded the Healthcare Technology Innovation Award, along with…

VitalStream offers continuous hemodynamic monitoring solution amid IV fluid shortage
Philadelphia, PA – October 9, 2024 – Caretaker Medical, a pioneer in advanced hemodynamic monitoring technology, is highlighting the critical role of its VitalStream solution…

BP cuff, A-line or VitalStream noninvasive hemodynamic monitor?
Should you use a blood pressure cuff, arterial line or VitalStream to monitor your perioperative patients? Learn the about the strengths and weaknesses of each….
Request a demo
See how VitalStream can improve the continuous hemodynamic monitoring experience for you and your patients.

- Kwon Y, Stafford PL, Enfield K, Mazimba S, Baruch MC. Continuous Noninvasive Blood Pressure Monitoring of Beat-By-Beat Blood Pressure and Heart Rate Using Caretaker Compared With Invasive Arterial Catheter in the Intensive Care Unit. J Cardiothorac Vasc Anesth. 2022 Jul;36(7):2012-2021. doi: 10.1053/j.jvca.2021.09.042. Epub 2021 Oct 1. PMID: 34666928; PMCID: PMC8971137.
- Khanna AK, Garcia JO, Saha AK, Harris L, Baruch M, Martin RS. Agreement between cardiac output estimation with a wireless, wearable pulse decomposition analysis device and continuous thermodilution in post cardiac surgery intensive care unit patients. J Clin Monit Comput. 2023 Jul 17. doi: 10.1007/s10877-023-01059-5. Epub ahead of print. PMID: 37458916.
- Salmasi V, Maheshwari K, Yang D, Mascha EJ, Singh A, Sessler DI, Kurz A. Relationship between Intraoperative Hypotension, Defined by Either Reduction from Baseline or Absolute Thresholds, and Acute Kidney and Myocardial Injury after Noncardiac Surgery: A Retrospective Cohort Analysis. Anesthesiology. 2017 Jan;126(1):47-65. doi:
10.1097/ALN.0000000000001432. PMID: 27792044. - Haraden C. Diagnostics for Patient Safety and Quality of Care. Patient Safety Executive Development Forum, Institute for Healthcare Improvement. 2014. https://cdn2.hubspot.net/hubfs/5599582/SoteraWireless-April2020/PDF/White-Paper-Surveillance-Monitoring-General-Care-Part-1-1.pdf
- Institute for Health and Care Excellence. Intravenous fluid therapy in adults in hospital – clinical guideline (CG174). https://www.nice.org.uk/guidance/cg174. Published December 2013. Updated May 2017. Accessed (August 20, 2020).
- Magee G, Zbrozek A. Fluid overload is associated with increases in length of stay and hospital costs: pooled analysis of data from more than 600 US hospitals. Clinicoecon Outcomes Res. 2013 Jun 26;5:289-96. doi: 10.2147/CEOR.S45873. PMID: 23836999; PMCID: PMC3699028.
- Child, Debra & Cao, Zhun & Seiberlich, Laura & Brown, Harold & Greenberg, Jordan & Swanson, Anne & Sewall, Martha & Robinson, Scott. (2015). The costs of fluid overload in the adult intensive care unit: Is a small-volume infusion model a proactive solution?. ClinicoEconomics and outcomes research : CEOR. 7. 1-8. 10.2147/CEOR.S72776.
- Kambiz Kalantari, Jamison N. Chang, Claudio Ronco, Mitchell H. Rosner, Assessment of intravascular volume status and volume responsiveness in critically ill patients, Kidney International, Volume 83, Issue 6, 2013, Pages 1017-1028, ISSN 0085-2538, https://doi.org/10.1038/ki.2012.424.
- Donald M. Yealy, Nicholas M. Mohr, Nathan I. Shapiro, Arjun Venkatesh, Alan E. Jones, Wesley H. Self. Early Care of Adults With Suspected Sepsis in the Emergency Department and Out-of-Hospital Environment: A Consensus-Based Task Force Report. Published: April 09, 2021. DOI:https://doi.org/10.1016/j.annemergmed.2021.02.006
